Early Roots: Plants as America’s First Medicines
Before there were pharmacies or prescription bottles, there were herbs, simple leaves, roots, seeds, and flowers, shared by Indigenous peoples and woven into everyday life by early colonists. Knowledge about healing plants like willow (for pain), goldenseal (for infections), and echinacea (for immune defense) was passed directly from Indigenous Americans to settlers looking for ways to survive and thrive in a new land.
Just to give you a sense of scale, by the early 1900s, about 40% of official medicinal preparations in the U.S. were crude plant extracts, and plants like cannabis were even included in the U.S. Pharmacopoeia, the “official” list of medicines, until well into the 20th century.

The Boom: Rise of Eclectic Medicine and Herbal Schools
Picture America in the 1800s. Medical care is all over the map, literally. Mainstream doctors (sometimes known as “regulars”) are bleeding people or prescribing mercury (not a great idea). But others, Thomsonians and Eclectics, are blending tradition and science using local plants and hands-on, holistic methods.
The Thomsonian Movement
This is the era of Samuel Thomson, a self-taught herbalist whose system of medicine is straightforward and accessible: use herbs, focus on sweat and “heat”, and avoid harsh chemicals. Ordinary folks embrace his ideas, growing and preparing their own remedies. “Thomsonian” medicine brings herbal healing into homes across the country.
Eclectic Medicine’s Scientific Approach
Out of this landscape grows the Eclectic movement. Led by Dr. Wooster Beach, Eclectic schools offer a middle way, combining scientific inquiry with traditional herbalism. Students at eclectic colleges, like the Reformed Medical College of the City of New York, study American native plants in detail, record their effects, and reject bloodletting and heavy metals.
Eclectics draw a thoughtful, research-minded crowd. They keep detailed “materia medica” guides describing plant properties and treatments, essentially laying the groundwork for what we now call evidence-based herbalism. By the late 1800s, eclectic medical colleges are scattered all over America, turning out doctors who combine modern diagnostics with botanical know-how.
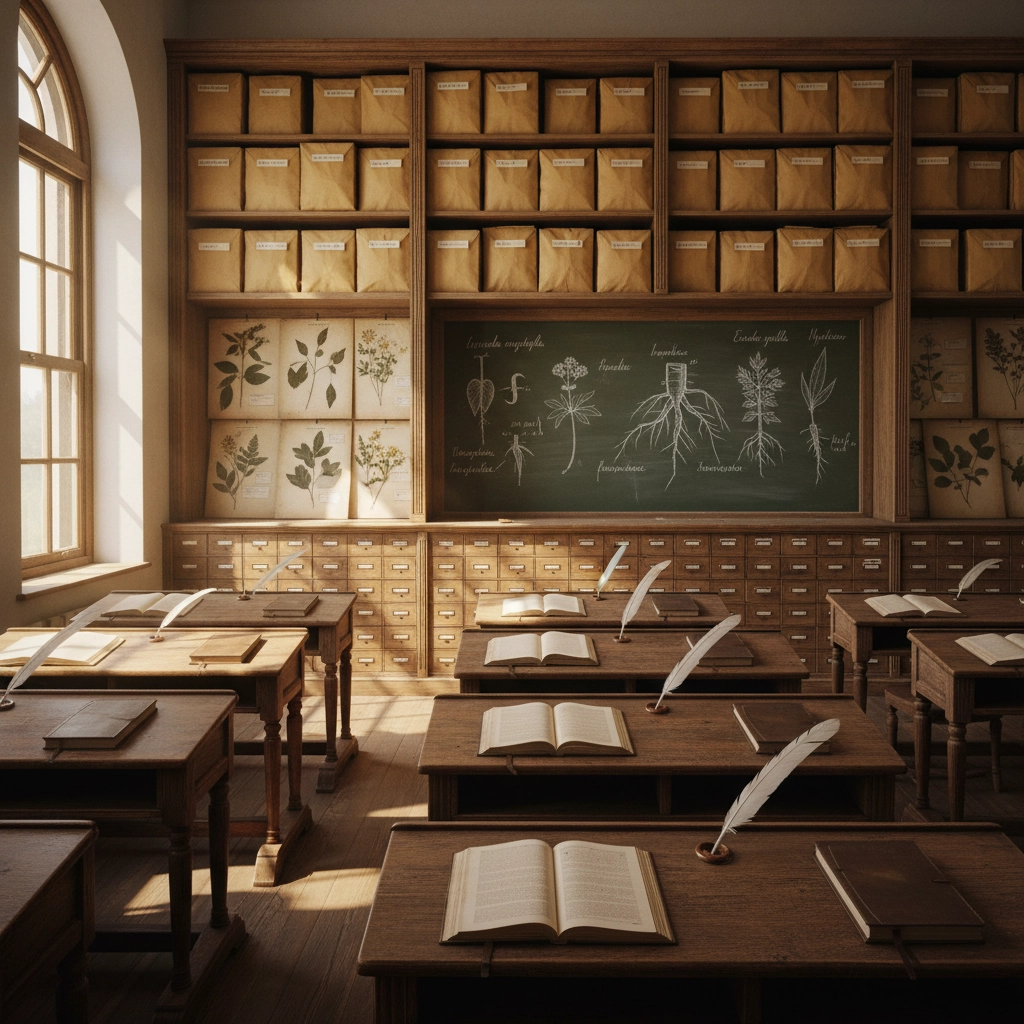
Practitioners in the Eclectic tradition believed knowing your plants mattered as much as knowing your patients.
The Crackdown Begins: The Flexner Report & Medical Standardization
Fast forward to the early 1900s. The American Medical Association (AMA) is on a mission to standardize and “upgrade” medical education. In 1910, the Flexner Report, a major investigation funded by the Carnegie Foundation, sends shockwaves through American medicine. The report’s bottom line: Medical schools should be housed in universities, focused on laboratory science, and should weed out “irregulars”, including herbalists, Eclectics, homeopaths, and women- or Black-led colleges.
The Impact
- Over half of all medical schools in the U.S. shut down or merged between 1910 and 1935.
- Herbal study is slashed from school curriculums. Students learn only “orthodox medicine”, the emerging pharmaceutical model focused on single-compound, laboratory drugs.
- Famous eclectic colleges close their doors; only allopathic (conventional) medical programs survive.
In just one generation, professional-level herbal medicine is pushed to the fringe. Mainstream doctors are no longer trained in plant-based care, and communities lose access to trusted, holistic practitioners.
“By 1934, the Eclectic Medical Association had essentially ceased to exist as a major force in American medicine.”
Modern Era: Regulation, Rebirth & Roadblocks
The FDA Enters the Scene
The Pure Food and Drug Act of 1906 requires patent medicines (secret formulas) to be fully labeled, cracking down on fraudulent claims and shifting the culture toward lab-tested drugs [and away from folk remedies]. By the mid-1900s, the U.S. Pharmacopoeia is quietly removing most herbal preparations from its listings.
In the second half of the 20th century, the FDA (Food and Drug Administration) has the final word on what is or isn’t a medicine. Today:
- All “drugs” must be proven safe and effective via rigorous clinical trials, a process that costs millions.
- Herbs and essential oils (unless specifically studied and approved) are usually classified as supplements or cosmetics.
- Companies can’t claim their products “prevent, treat, or cure” disease without FDA approval.
Herbs Today: Restricted But Resilient
Ever wonder why your favorite herbal tincture has that little asterisk and says “This statement has not been evaluated by the FDA”?
It’s because even though herbal medicine has deep roots in American history, the laws are stacked in favor of single-compound pharmaceuticals. FDA policy does not regulate the practice of medicine, your physician can still recommend (or avoid) herbs as they see fit, but for companies, it’s a long and costly road to get herbal formulas officially recognized as “medicine.”
Why Isn’t the U.S. Fully Aligned with Herbal Medicine?
Despite a wellness movement and renewed interest in “natural” products, the U.S. system remains out of sync with herbalism, for a few key reasons:
1. Medical Education Gaps
Doctors in the U.S. rarely receive significant training in nutrition, herbal medicine, or holistic wellness, unlike their counterparts in China or parts of Europe. If it’s not in the medical curriculum, it’s less likely to make it into mainstream healthcare.
2. Pharmaceutical Model Dominance
The American drug approval process is designed for isolated, standardized chemicals (think: ibuprofen) rather than complex, multi-compound plants (think: willow bark). As a result, research and insurance coverage both favor pharmaceuticals.
3. Regulatory Hurdles
Large-scale clinical trials, which are required for any health claims, can be prohibitively expensive for small herbal companies and farmers. That’s why most herbal products in stores are labeled for “support” or “wellness,” not for actual treatment.
4. Skepticism and Misinformation
Centuries of advertising, shifting laws, and periodic “snake oil” scandals have trained the public to view herbal medicine with skepticism, especially when scientific studies seem to offer mixed results.
5. Consumer Confusion
In the U.S., herbal products are regulated as dietary supplements, which means quality, potency, and purity can vary widely unless you buy from transparent, reputable brands.

(AEtherbal’s commitment: transparency, high quality herb sourcing, and inspired by historic traditions, visit our shop for more!)
Is History Repeating Itself?
Interestingly, while China reintegrated herbal training into medical schools in the 20th century, teaching thousands of practitioners each year, the U.S. largely moved herbs out of its mainstream. The result? Most American herbalists today learn outside the university system: through independent schools, apprenticeships, or even self-study.
But tides are changing. There’s renewed interest in “root medicine,” holistic care, and integrating ancient wisdom with modern science.
What’s Next for Herbalism in America?
While the FDA and U.S. law will likely keep herbs labeled as “supplements” for the foreseeable future, demand for quality, transparency, and real results is rising. Whether you’re new to herbs or getting back in touch with your roots, there’s a whole world of plant wisdom waiting to be rediscovered.
At AEtherbal, our mission is simple: honor traditional herbal knowledge, use only top-grade botanicals, and help you make informed decisions about your health, naturally.
Please consult with your physician prior to starting any herbal remedy. These statements are not meant to diagnose, treat, or cure any illness.





